
Medicaid is a microcosm of political debate in the United States. Historically, it stokes the fires deep within both political sides. For liberals, it is a grand, Great Society-era program designed to support the health of our society’s most needy. For conservatives, it is an example of the worst kind of federal program; it is unearned, unwieldy, and susceptible to waste and abuse.
In contemporary politics Medicaid is at the center of several of the most contentious elements of the Affordable Care Act (aka Obamacare). Liberals view it as a model for universal healthcare. Conservatives view it as emblematic of government’s inability to effectively address individual needs.
On the individual level, Medicaid is also representative of why a lot of people struggle to engage in politics: it is complicated; it is full of regulations; and it is highly variable from state to state, meaning understanding Medicaid in North Carolina does little for understanding Medicaid in Wisconsin. It is the type of policy issue that everyone should understand but almost no one fully does. On a personal level, articles on Medicaid are the ones that I mark to read later and never do.
One of the goals of Insight is to help identify and easily synthesize topics that are not necessarily front page material but that our team believes should be on the radar. Enter the N.C. Department of Health and Human Services’s (DHHS) Proposed Program Design for Medicaid Managed Care.
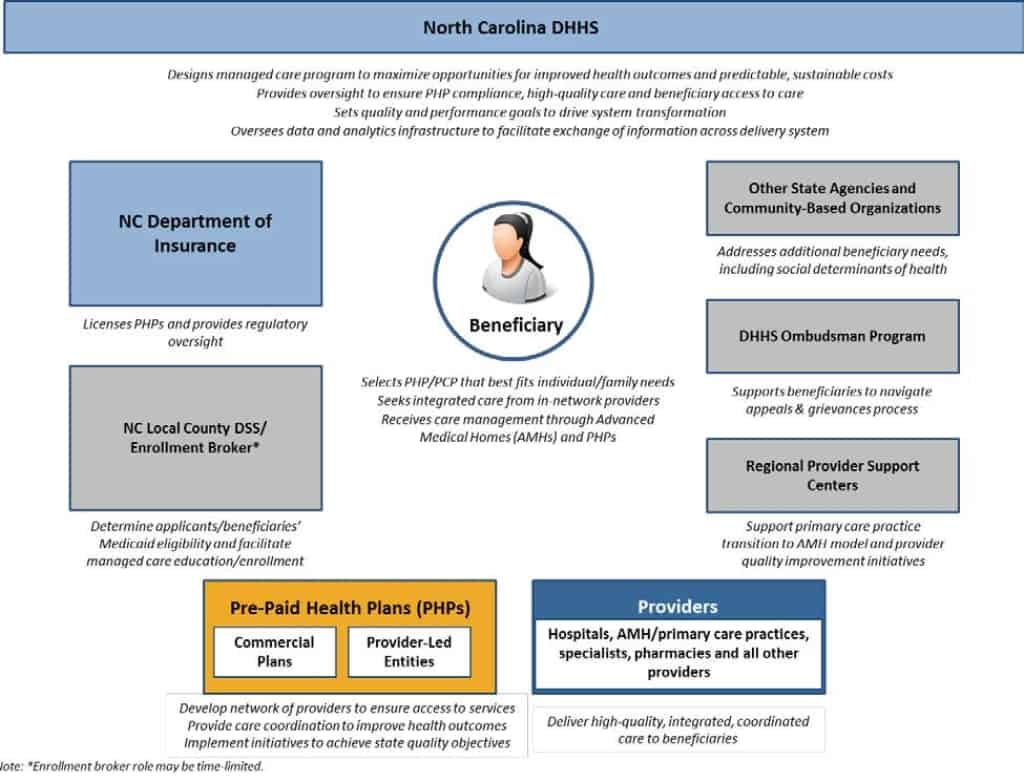
Roles and Responsibilities of Key North Carolina Stakeholders under Managed Care
Background
According to the Kaiser Family Foundation’s Medicaid Fact Sheet on North Carolina, 18 percent of the population is covered by Medicaid or the related Children’s Health Insurance Program. Specifically, Medicaid serves the following sub-sections of the populations in N.C.:
- 1 in 8 adults younger than 65
- 2 in 5 low-income individuals
- 2 in 5 children
- 3 in 5 nursing home residents
- 2 in 5 people with disabilities
At the end of the 2015 legislative session, the General Assembly passed legislation that changed the way Medicaid and the related Health Choice program operate in N.C. The legislature instructed DHHS to construct reforms that target four goals:
- budget predictability attained through shared risk and accountability;
- balanced quality, patient satisfaction, and financial measures;
- efficient and cost-effective administrative systems and structures; and
- a sustainable delivery system attained through the establishment of provider-led entities and commercial prepaid health plans (PHPs).
In moving towards those goals, DHHS began the planning process to move from a fee-for-service model of care delivery to a managed care model. In a fee-for-service model, patients pay for medical services as they receive them. This creates an incentive for patients and doctors to treat medical conditions as isolated incidents rather than part of each patient’s broader health experience.
Managed care, on the other hand, tries to focus on the entire patient. It creates incentives for medical care providers, health administrators and individuals to take preventive measures that improve overall health results. Here is a brief description of a managed care model from the Patient Advocate Forum:
Managed care is the prevalent system through which health care services are coordinated and delivered today. This system provides a broad range of health insurance products available to consumers. Managed care integrates the payment and delivery of health care products and services to consumers in an effort to deliver the highest quality services at the lowest possible cost.
For additional background on recent Medicaid reform efforts in North Carolina, see the N.C. Medical Journal’s January, 2017 overview and the Kaiser Family Foundation’s Fact Sheet on Medicaid Delivery System and Payment Reform.
Moving Forward
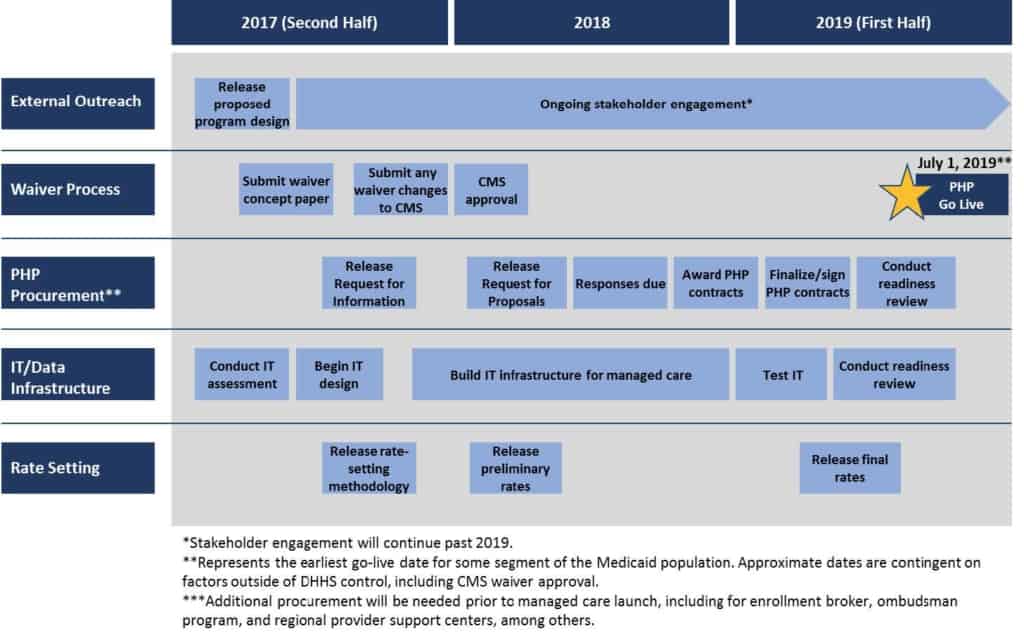
On August 8, DHHS released a detailed overview of the proposed changes to Medicaid administration in the state. The overview offers an initial sense of the focus points of the programs, the incentive structure and the timeline. The implementation of the managed care model is scheduled to evolve through the first half 2019, with various special populations moving to the new model in the succeeding four years. DHHS is seeking comments on its proposal through September 8, 2017. DHHS’s timeline for the project is below.
Sequencing of Key Activities to Launch Managed Care
What is significant
The DHHS overview document is readable and focused on outlining the conceptual shifts in the program. Summarizing it is providing an overview of the overview. However, several noteworthy shifts stand out.
1) The crux of a managed care system is the shift to prepaid health plans, which shifts the risk from the payer to managed care provider. The proposed system in N.C. will include two sub-systems: statewide commercial plans and regional provider-led entities. As provided in the reform legislation, the state will offer three commercial plans that must serve the entire state. In addition, the regional provider-led options will be designed within one of six regions.
2) The proposed Managed Care system seeks to integrate the delivery systems for physical health services, behavioral health services and intellectual and developmental disability services. Currently, these services are not paired, which can lead to inefficiencies in patient care due to lack of coordination. Additionally, the program will provide “tailored plans” designed for patients with unique health care needs.
3) DHHS intends to hire a broker who will work with beneficiaries in choosing the right managed care provider.
4) The proposal specifically notes the interaction between the state’s opioid abuse problems. Beginning this year, DHHS will reduce the permitted maximum daily dosage of opioids. In addition, the new Medicaid administration is considering multiple strategies to treat and prevent opioid abuse.
5) DHHS has proposed a strategy to assess and incentivize quality in serving Medicaid beneficiaries across the different managed care providers with the hope of reducing costs and improving outcomes over time.
Share your thoughts
Officially, DHHS has asked for feedback on the proposal by September 8, 2017. The email address is Medicaid.Transformation@dhhs.nc.gov. For any interested in sharing less formal feedback, the Center will open up the comments section on this post and share with DHHS by the deadline. In addition, we have partnered with our friends at Reach NC Voices and have initiated this simple survey poll to gauge general thoughts on Medicaid. Tell us what you’re thinking.
Weekly Insight Health & Human Services


