
“We have the State Crime Lab under the Department of Justice, and I was in the lab one day watching a drug chemistry scientist test a batch of heroin that had been sent in by a local law enforcement agency,” said N.C. Attorney General Josh Stein.
“She was showing me how she tested different packets. Some would have a little fentanyl and some would have a lot of fentanyl, and it’s because you have these garage chemists mixing drugs, and there’s no consistency with what they put in it,” Stein said.
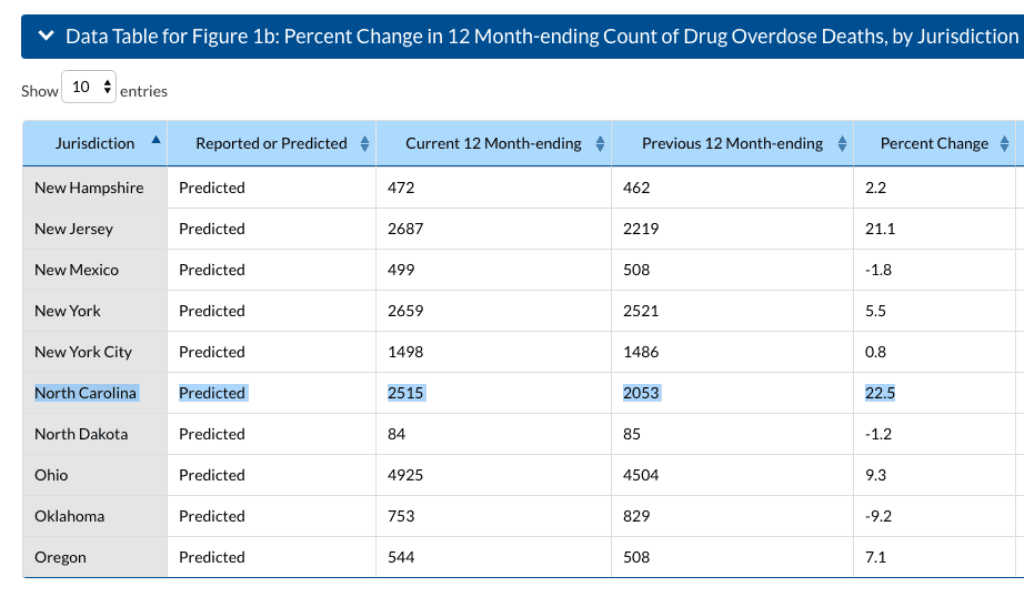
These variable amounts of fentanyl—a synthetic opioid with 100 times the potency of morphine—prove fatal and are responsible for a surge in overdose deaths across the state. According to a report released last month by the Centers for Disease Control and Prevention (CDC), North Carolina has one of the highest predicted percentage increases in overdose-related deaths in the country for 2017-2018 at 22.5 percent.
“Essentially, there are three buckets of opioids that are killing people. There are the prescription pills—the traditional notion of the pain killers. Then you have heroin, a street drug. And then you have the fentanyl, which is also a street drug,” Stein said. “In the last two to three years, there has just been a skyrocketing of people dying from heroin, but in particular the synthetic drugs.”
Stein said drug traffickers and dealers prefer lab-made fentanyl because it’s substantially cheaper to manufacture than it is to grow and import heroin. Also of concern, traffickers have used fentanyl to cut more than just heroin. Overdoses due to fentanyl have been found in people who used cocaine or marijuana without knowing their drugs were laced with the synthetic opioid.
That fentanyl is becoming much more than heroin or opioid-related is also evident. Vox published an article earlier this year titled “Why America’s cocaine problem is now a fentanyl problem too.” Meanwhile, the issue of increased trafficking of fentanyl isn’t at all unique to North Carolina. The CDC reported last year that overdose deaths due to “fentanyl and variations of the drug nearly doubled” with an alarming rise from Philadelphia to Chicago—and let’s be honest, throughout the entire country.
TERRIFYING STATISTIC: There was a 25% increase in opioid-related poisoning deaths last year in NC over 2016, according to DHHS provisional data. With 1,584 opioid overdose deaths, 2016 had been the state’s deadliest year yet. In 2017, that number skyrocketed to 1,974 deaths.
— Josh Stein (@JoshStein_) August 23, 2018
But with North Carolina among the highest projected increases in overdose deaths, what is the state doing about it?
“On prevention, we’re making progress. We’re seeing a dip in the number of pills that are being prescribed by doctors, which will have the long-term benefit of having fewer people becoming addicted, so over time we will see a reduction in addiction,” Attorney General Stein said. “On enforcement, we’ve been working with law enforcement to give them access to tools and strategies to more effectively confront the crime in their communities. But I think until we solve the treatment issue and actually provide more health care to the people who need it, we will continue to see a lot of deaths.”
The big picture
The United States witnessed more than 70,000 overdose deaths last year: a record high. As for our piece of that puzzle, the North Carolina Department of Health and Human Services (DHHS) data for 2016 reports over 2,100 overdose deaths (and not just by opioids) across the state. (See the interactive visualization for 2016 numbers below. County-by-county data for 2017 will be released by DHHS in a few weeks.) However, the “public health opioid epidemic”—while certainly tied to potent synthetic variants like fentanyl—continues to rise nationwide because of its complexity.
The crisis is not simply a prevention problem, or a law enforcement problem, or a prescription problem, or a treatment problem. Each contributing factor of the epidemic is part of a perfect storm that has birthed addicted babies and made grandmothers mothers to their grandchildren.
When I served as Interim Managing Editor of the North Carolina Medical Journal (NCMJ), a publication of the N.C. Institute of Medicine, we took on the daunting task of dedicating an issue of the journal to the opioid crisis. In our first planning meeting with guest editors Secretary Mandy Cohen and Susan Kansagra of DHHS, there was enough ground to cover to easily fill two of the 76-page journal issues. After several difficult editorial cuts, we decided to align articles with DHHS’ Opioid Action Plan. Below are points of the action plan and summaries of some the journal articles that address them.
DHHS Action Plan: Coordinating the state’s infrastructure to tackle the opioid crisis.
NCMJ Article: The Opioid Epidemic in NC: Progress, Challenges, and Opportunities by Mandy Cohen and Susan Kansagra
Like many states, North Carolina faces an opioid crisis that has rapidly intensified in recent years. Addressing this epidemic requires interventions such as judicious prescribing of opioids, community based prevention efforts, broader naloxone distribution, law enforcement efforts to curb drug trafficking, and harm reduction efforts like safe syringe programs. Expanding access to treatment and recovery services, as well as affordable health insurance for individuals with substance use disorder or at risk for developing a disorder, is also critical. North Carolina has made significant progress, but we have much more work to do.
DHHS Action Plan: Reducing the oversupply of prescription opioids.
NCMJ Article: Reducing the Oversupply of Prescription Opioids by Sara McEwen and Steven Prakken
Prescribers have played an important role in the development of the opioid epidemic. Efforts to reduce the oversupply of prescription opioids are underway in the form of guidelines and legislation. Such efforts must be part of a larger public health approach that supports best practices and access to addiction treatment.
DHHS Action Plan: Reducing the diversion of prescription drugs and the flow of illicit drugs.
NCMJ Article: How Did We Get Here? Heroin and Fentanyl Trafficking Trends: A Law Enforcement Perspective by Leslie Cooley Dismukes
Illicit heroin and fentanyl are infecting North Carolina’s communities, and causing an increasing number of overdose deaths. These trends in drug trafficking and opioid misuse represent a dramatic shift, necessitating a new and coordinated law enforcement response. The North Carolina Attorney General’s Office is committed to working toward increased enforcement, prevention, and treatment to address this epidemic.
DHHS Action Plan: Increasing community awareness and prevention.
NCMJ Article: Fighting the Opioid Epidemic in North Carolina with Leadership, Compassion, and Creativity: Community Approaches by Lisa Macon Harrison and Fred McClure
Our state’s motto is “Esse quam videri – To be rather than to seem.” North Carolina struggles with insufficient systems to adequately address the opioid crisis we are experiencing. However, progress is happening. Leaders are making a difference across organizations, partnerships, and communities large and small. Where there is a will, North Carolina people are finding creative solutions to address the opioid crisis and its underlying health issues. We cannot wait. We cannot seem. We cannot be afraid.
DHHS Action Plan: Making naloxone widely available.
NCMJ Article: Harm Reduction Strategies for the Opioid Crisis by Tessie Castillo
In order to reduce disease transmission and overdose death resulting from the opioid crisis, North Carolina has recently adopted several harm reduction programs, including community based naloxone distribution and syringe exchange. Additionally, discussions are taking place about safe injection facilities as a way to further reduce the harm of opioids.
DHHS Action Plan: Expanding treatment and recovery systems of care.
NCMJ Article: Opioid Use Disorder: Treatment & Recovery by Smith Worth and Kenny House
The current opioid epidemic is devastating to the lives of individuals, families, and communities, but there are effective treatment approaches available. Treatment that combines proven medications with behavioral therapies and other supports is giving many in North Carolina the opportunity to engage in successful recovery.
DHHS Action Plan: Measuring the effectiveness of these strategies based on results.
NCMJ Article: County Level Dynamics of Heroin Mortality in North Carolina by Duke Institute for Brain Sciences
In North Carolina, the number of opioid overdose deaths has increased by nearly 800% between 1999 and 2016. Prior to 2010, over two-thirds of opioid deaths were the result of prescription opioids, but since 2013, prescription opioids have been responsible for less than 45% of opioid overdose deaths, and opioid deaths by illicit drug use have increased dramatically. One goal of North Carolina’s Opioid Action Plan from June 2017 is to reduce the number of deaths from opioid overdose by 20% by 2021. County level mortality trends must be examined to effectively deploy resources to achieve this goal. This analysis characterizes the dynamics of the opioid epidemic with regard to heroin overdose deaths in North Carolina. The purpose of our analysis is to investigate whether there is variation in the pattern of heroin mortality among counties and identify counties within North Carolina that may be used to inform both potential solutions and areas of greatest need.
The journal also took on adverse childhood experiences as a major contributor to the crisis and examined addiction as a chronic illness. (You may view the full opioid journal issue released in May, here.)
“This is a crisis that is long in the making. It’s taken us about 20 years to get to this stage of crisis, and we are not going to solve the problem in 2018 or even in 2019,” Attorney General Stein said. “It’s going to require many different types of people—from health care to law enforcement to policymakers to the business community—all working together in a concerted fashion for us to turn the tide on this. When we do that, I’m confident that we can have success and we can save lives.”
Weekly Insight Health & Human Services

