
The story of health care in the United States today is one of consolidation. Whether the headlines of the day address another merger of giant health systems, such as the proposed merger between UNC Health Care and Atrium or the much-anticipated alliance of Amazon, JP Morgan, and Berkshire Hathaway to tackle the health care costs of their employees, the narrative arc of the health care universe bends towards amalgamation.
But the story is not about industry giants but about a similar phenomenon in the public sector: the standardization and streamlining of health provider licensing regulations across states.
The regulation of professional health care providers is recognized as an exclusive (and jealously guarded) state power. It has also been the subject of some criticism as an unnecessarily burdensome and duplicative process.
However, in response to the growing need for provider mobility in order to address widening disparities in access for rural communities, states are voluntarily aligning regulatory requirements and enforcement. One example of this is the Enhanced Nurse Licensure Compact, which North Carolina entered this past summer.
What it is
The Enhanced Nurse Licensure Compact is a multistate practice license allowing nurses to practice in any of 29 participating member states. Created in 1998, the Compact got a big boost this past year when North Carolina and 25 others states joined the coalition (re-upping their membership from the original, smaller Compact confederation).
Under this program, nurses licensed in North Carolina who meet 11 uniform licensure requirements are entitled to this multistate license, authorizing them to practice (physically, electronically and telephonically) across state borders and serve patients located in other member states. In doing so, the nurse must comply with the practice rules and regulations of the state in which care is provided; however, only the “home” state has authority to take disciplinary action in the event of a complaint or alleged violation.
Founded in 1998, North Carolina was one of the first members of the original, more limited Compact, which represented a looser coalition among a smaller number of states granting reciprocity. The enhanced model significantly expands the pool of member states and provides greater digital coordination and clarity regarding the home state’s exclusive disciplinary authority.
While the Compact represents the first model for interstate licensure in the healthcare profession, it is not the last: there is a similar Interstate Medical License Compact in operation in 22 states and a recently founded Physical Therapy Licensure Compact.
Why it is important
Nursing has been at the forefront of multistate licensure. This “radical” departure from the status quo of licensing boards is in response to big challenges facing states including maldistribution of health care resources and providers between rural and urban communities, more commonly referred to as the rural health crisis.
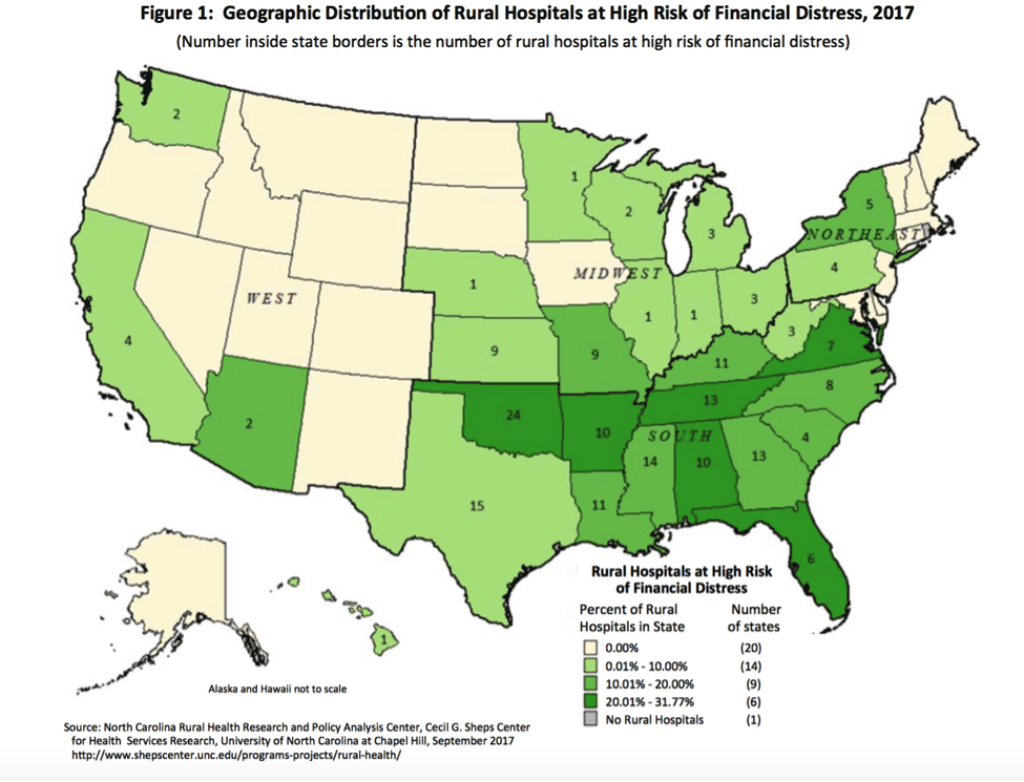
North Carolina made national headlines with the closure of five rural hospitals in the past seven years. As reflected in the graphic created by the Cecil G. Sheps Center for Health Services Research below, North Carolina, like many of its neighboring southern states, has a high incidence of hospitals at high risk of financial distress and possible future closure. North Carolina is home to 147 federally-designated Primary Care Health Professional Shortage Areas, and the majority of those are in rural counties.
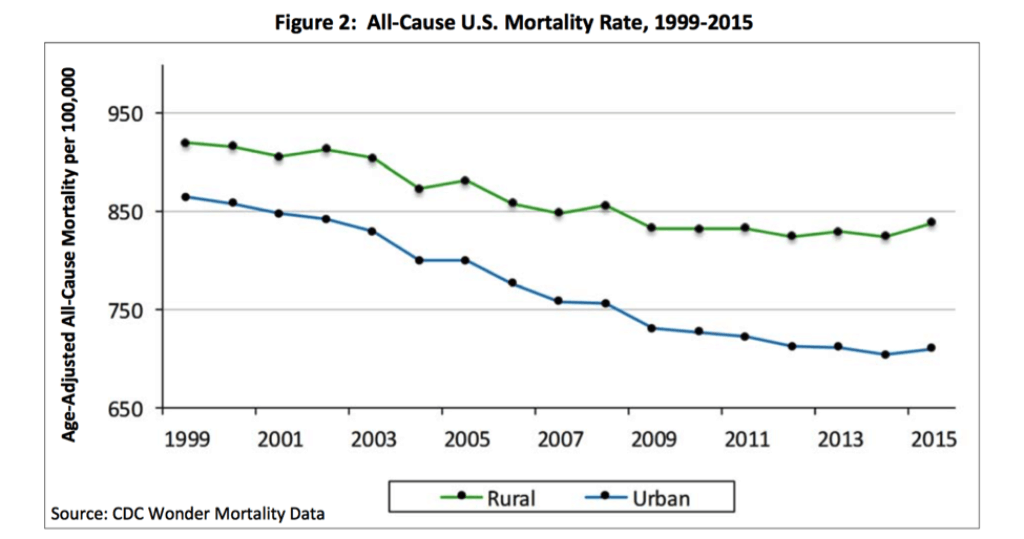
This disparity in access to providers translates to poor outcomes for rural residents. As Mark Holmes, director of the Cecil G. Sheps Center for Health Services Research at UNC-Chapel Hill, explained to North Carolina Health News last month:
“Almost any measure you look at in terms of rural health, rural areas are doing poorer….They’re older. They’re poorer. They’re most isolated. They have persistently higher mortality on just about every indicator you look at… from the prevalence of diabetes to opioid use.”
Telemedicine is one tool legislators and state agencies have identified to assuage this problem, and the establishment of a multistate licensure process addresses one of the biggest practical barriers to the use of telemedicine.
The importance of telemedicine in bridging the care gap in underserved communities is hard to overstate. The North Carolina DHHS identified telemedicine as a central strategy to reach the most vulnerable residents in North Carolina – particularly in primary care and in delivering psychiatry and behavioral health services. The Department has specifically recommended adoption of a similar compact license for physicians in the coming year.
Read more about telemedicine in the Center’s 2014 North Carolina Insight, Evaluating Mental Health Reform in North Carolina.
Where we go from here
In the age of increasing corporatization and consolidation, there is concern about the diminished capacity of the state to regulate activities around public health and safety of its citizens. Imposing uniform qualification requirements streamlines the process to practice, removing administrative obstacles while preserving the authority of the state to regulate the substance.
Regulating process and administrative procedures is easier, but quality outcomes are what matter. It is still early, but time will tell if state boards are able to manage substantive enforcement of regulatory standards and board complaints across jurisdictions.
Weekly Insight Health & Human Services

