 On Sunday, October 16th, North Carolina Health News as part of their Lives on the Hill project, held a community convening to talk about how to preserve the legacy of Dorothea Dix Hospital. The gathering brought together people whose lives were affected by the hospital – patients and their families, former staff and their families, neighbors, and other interested citizens.
On Sunday, October 16th, North Carolina Health News as part of their Lives on the Hill project, held a community convening to talk about how to preserve the legacy of Dorothea Dix Hospital. The gathering brought together people whose lives were affected by the hospital – patients and their families, former staff and their families, neighbors, and other interested citizens.
The N.C. Center for Public Policy Research has conducted extensive research on North Carolina’s efforts in mental health reform including The History of Mental Health Reform, The State of Mental Health Reform, and Evaluating Mental Health Reform.
Former NCCPPR director of law and policy and editor of N.C. Insight, Mebane Rash, a speaker at the event, talked about the history of Dix Hospital, the humanity of mental health, and the N.C. Center’s research on mental health policy.
Below are her remarks:
Today we are here to think and to dream about the essential humanity of mental health as an important public policy issue but also as a lived reality for many of us.
This is an issue that touches all of our lives, and today – thanks to NC Health News – we have an opportunity to think about how to connect our past to the future.
In March 2009, the N.C. Center for Public Policy Research published an in-depth look at the history of mental health reform in North Carolina. It won a national award for most distinguished policy research because we believed that history can help illuminate public policy in ways that will inform change. The stories of people impacted by this issue – those with mental illness, change agents like Dorothea Dix, and policymakers – have to be remembered to build public will and legislative commitment going forward.
“Historical knowledge can deepen the way in which we think about contemporary issues and problems. It can also sensitize us to the dangers of simplistic solutions.”—Gerald N. Grob, Ph.D.
As I share with you some of the stories that led us to this day, here is the policy context. Our review of the evolution of mental health policy in this state illustrates that regardless of the time and nature of the reform, there are complex and not easily resolved core issues: (1) governance – which government entity has responsibility for the welfare of the mentally ill; (2) coverage – which individuals should be included in government-provided mental health care and what services should be provided; (3) funding – how will the necessary services be paid for; and (4) work force – who will provide the treatment?
During the early 1800s, often those with mental illness who could not be cared for at home were housed in jails. The March 14th, 1803, edition of The Raleigh Register tells the story of Christian Brown. The Salisbury jail was brand new. It had scarcely been finished. It housed four prisoners, and one man, Christian Brown, suffering from insanity, as it was called at the time. When flames were discovered at midnight, the fire had gathered such force that it could not be contained or put out, and the building burned down to the stone walls. The four prisoners were awakened by the cries of the insane man, and they escaped unhurt. Christian Brown died in the fire, chained in the jail. But for the accident which destroyed him, physicians were of the opinion he would have recovered the use of his reason.
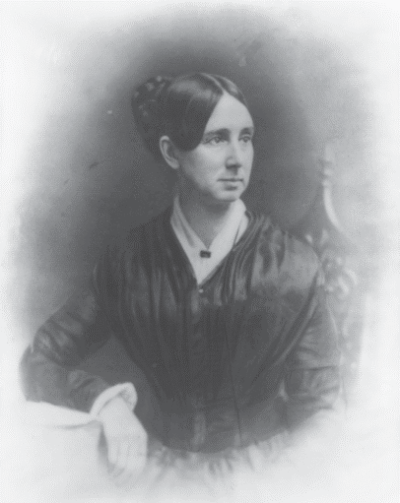
Thirty eight years later, in 1841, a woman named Dorothea Dix visited an East Cambridge, Massachusetts jail, where she was shocked to see those with mental illness treated as criminals and “chained, naked, beaten with rods and lashed into obedience.” Her crusade was born, and in 1848, Dix came to North Carolina. Here is how she described the situation in Lincoln County: “Near a public road … is a log cabin strongly built, about 10 feet square, about seven or eight feet high; no windows to admit light … no chimney indicates that a fire can be kindled within, and the small low door is securely locked and barred . . . You need not ask to what uses it is appropriated. The shrill cries of an incarcerated maniac will arrest you on the way.” Dix urged our legislature to establish a hospital for the mentally ill.
By 1849, the General Assembly appropriated the money, and by 1856, Dorothea Dix Hospital opened atop the rolling hills of former farmland here in Raleigh. Mental health reformers like Dix undertook to build a system of public mental health hospitals to care for and treat citizens with severe and persistent mental disorders.
But the asylum movement fell short for the systemic reasons I mentioned – Governance and coverage: Local governments were unable to provide services for those who could be treated locally and this led to overcrowding at state institutions. Work force: With staff shortages, high turnover, poor working conditions, and inexperience. And funding: As asylums had to deal with delinquent payments from localities and inadequate state appropriations.

The history of reform shows that improving the treatment and care of the mentally ill is a complex process that has evolved incrementally – sometimes with major leaps forward followed by substantial retreats.
In the 1960s, there was a nationwide move towards deinstitutionalization, an effort to move those with mental health issues – whether mental illness, intellectual disabilities, or substance abuse – out of state institutions and into local, community-based treatment settings. Our state struggled to figure out how many beds at state psychiatric hospitals would be enough.
Kenneth C. Royall, Jr., served in the state House and later in the Senate from 1967 to 1992. He “was known for his intimidating girth, his growl of a voice and his fierce command of the state’s budget – all of which led to his nickname, ‘The Bear,’” wrote columnist Ruth Sheehan in The News & Observer. But when it came to mental health, Sen. Royall was more of a teddy bear.
Royall’s son recalls driving with his dad past Cherry Hospital, one of the state psychiatric institutions. The father recounted to his son why it was important to him to take members of the budget committee to visit the hospitals. “‛Before we allocate any money for the state, … We’re going to tour the mental health care facilities and those facilities where people cannot care for themselves. … We are going to take care of these people first.’” Royall and his appropriations committee visited all of the state psychiatric hospitals in North Carolina. I wonder how many of the candidates in this election have visited even one of our state psychiatric institutions.
In the 1990s, as part of the team of Carolina Legal Assistance, a mental disability law project, I represented consumers being treated at Dix. For many Dix was a safe haven, a place to live life. I represented a teen who wanted to start a rock band. I represented those with intellectual disabilities that were being treated as if they were mentally ill – and the hospital worked to learn to provide appropriate support for them. The historic photos of Dix hospital remind us that people lived there, they worked there, they went to church there, they were buried there. They brought their suitcases to this place, and for many it was home.
In 1999, the U.S. Supreme Court handed down the Olmstead decision, which said required states to place persons with mental disabilities in the least restrictive setting possible and in community settings rather than in state institutions. And in 2001, North Carolina passed mental health reform legislation. Funding for mental health services more than doubled but 90 percent of it was spent on community support, and only 5 percent was spent on the seven services more likely to reduce the need for hospitalization.
“Health organization and policy never arise anew. They evolve from prior culture and understandings, health care arrangements, health professional organizations, and political and economic processes.”—David Mechanic, Ph.D.
In 2006, a 47-year-old man named Johnnie Yarborough was suffering from bipolar disorder and addicted to crack cocaine. He was so desperate for treatment that he beat on the doors of Dix Hospital. He was admitted to Dix 14 times during 2006, but never for more than a few days. Long-term care of the mentally ill became a thing of the past.
Over two hundred years after the death of Christian Brown, another man suffering from mental illness died in the state’s care. On April 29th, 2008, Steven Sabock, age 50, died at Cherry Hospital in Goldsboro. Sabock, who was being treated for bipolar disorder, was left overnight in a chair for 22 hours and 34 minutes in the hospital’s day room without food, water, or access to a bathroom before he died of a heart condition. In the security video, health care workers can be seen playing cards, watching television, and talking on cell phones.
The adult admissions ward was closed. An independent hospital management team was brought in. DHHS notified all state-operated facilities of a zero tolerance policy regarding the abuse and neglect of patients. “No abuse: not now, not ever” was the promise. Which begged the question, shouldn’t that have been our policy all along?
The role of psychiatric hospitals was reconsidered and the state begin to purchase beds in local hospitals across the state. This created funding pressure for the hospitals. Dix hospital closed.
The mother of a young girl, Brianna, told me once that for some, treatment in a state psychiatric hospital will always be needed. Now, as children wait in emergency rooms across our state for beds to open up, Brianna’s mother tweets every hour on the hour to state legislators often for days at a time. The wait is too long.
“‘The emphasis must be moved away from programs and places toward the patients themselves.’ We remain entrenched in our concerns about locus of care, confusing it with the humaneness, effectiveness, and quality of care.”—Jeffrey L. Geller, MD, MPH (quoting L.L. Bachrach)
Governance. Coverage. Funding. Workforce. Our public policy choices over time impact the lived realities of people we want to remember now as we think about the future – the lives lived on this hill can and should inform public policy in the 21st century.
Mark Long saw it all in his 30 years as a consumer of mental health services in North Carolina. He was admitted to every state psychiatric hospital, including Dix Hill. He lived in group homes and on the street. He tried nearly every treatment available.
Diagnosed with paranoid schizophrenia as a young man, Mark spent most of the 1970s and 80s in and out of psychiatric hospitals. Of the shift to community services in the 90s, he said, “I felt like a yo-yo. I would bounce into one situation and then I would bounce back out. I went from being in a hospital to being back in the community every few months.”
After making a third attempt to take his own life, Mark Long left the family care home where he was living, walked down the street, and found Residential Treatment Services of Alamance.
After he learned to live independently, Mark enrolled in UNC-Greensboro, graduating with a degree in social work. He became one of the first peer support specialists in our state.
Mark says, “To the people I work with, I can be as important as someone with a master’s degree in social work or a psychiatrist. It’s my life and experiences that allow me to connect with consumers in a different way and offer the kind of help another professional can’t.” Mark Long finally found the right treatment, a place to call home, and a vocation. He is a leader, having served on the State’s Consumer and Family Advisory Committee. His community-based treatment is his community-based life.
“One of the reasons why history repeats itself is because every generation refuses to read the minutes of the last meeting.”—Anonymous
History has much to teach us about our efforts to reform the mental health system in North Carolina since Dorothea Dix charted this path. The stories remind us of the public in this important public policy, like Christian, Johnnie, Steven, Brianna, and Mark. For me the lesson learned is that empowering consumers will lead to stronger, more enduring public policy solutions.
It will take all of us – family members, advocates, providers, funders, and policymakers working with consumers – to build a lived experience going forward that Dorothea Dix would be proud of.
Mebane Rash is the CEO and Editor-in-Chief of the online EdNC.org, which features nonpartisan news, research, data, and analysis on all things K-12 in North Carolina. She is a North Carolina native and an attorney in both the N.C. and federal court systems. For much of her career, Mebane worked at the nonpartisan N.C. Center for Public Policy Research as director of law and policy and the editor of N.C. Insight, the Center’s journal. During her time at the Center, she lead extensive research on North Carolina’s mental health system and advised lawmakers on mental health policy.
Read the Center’s full report on The History of Mental Health Reform here 
Read the Center’s report on The State of Mental Health in NC here 
Read the Center’s report on Evaluating Mental Health Reform in NC here
Mental Health

