Students in the Master of Public Policy program at Duke’s Sanford School of Public Policy spent part of their spring semester examining a policy issue for the N.C. Center for Public Policy Research.
The students investigated Alzheimer’s disease in North Carolina, looking at the rates of the disease, caregiving options for patients, and also looked to other states to learn about different options for comprehensive plans.
The students’ report, which includes recommendations for action in our state, is presented in this series of blog posts. The first part, posted today, provides an introduction to Alzheimer’s disease and an overview of prevalence rates.
Note: The pictures used in this series are from the Alzheimer’s North Carolina organization, a nonprofit dedicated to education, support, and advocacy for Alzheimer’s patients and their families. Visit their website here: http://www.alznc.org/ |
Alzheimer’s in North Carolina: Addressing Current and Future Needs
John Cubine, a 62-year-old man living in Kentucky, is a caregiver for his wife of 43 years, 62-year-old Gwen. She suffers from early-onset Alzheimer’s disease. Formally diagnosed seven years ago at age 55, Gwen started showing symptoms a year or two beforehand. Gwen has been given about two years to live and is close to requiring full-time care as her physical abilities decline. “If we weren’t fortunate enough to have resources, I would be trying to work and putting together caregivers on [an] ad hoc basis,” explains John. “I was lucky, I had enough time to retire and take care of Gwen full time. Otherwise finding a caregiver is tough – cost, dependability, background checks, etc. are all important considerations.”1
John says that one of his greatest challenges is to realize that his life has changed forever. He had to leave a job he loved and has now spent a tenth of his life as a caregiver. “Friends go away, not because they are mean or don’t care, but they can’t keep up the ‘death vigil’ for years. Life moves on.” John and Gwen are just one example of millions of people affected by Alzheimer’s disease in this country. Public policy interventions will be necessary to alleviate the hardships experienced by people like John and Gwen, until an effective cure is found for this horrific disease.
“I was lucky, I had enough time to retire and take care of Gwen full time. Otherwise finding a caregiver is tough – cost, dependability, background checks, etc. are all important considerations.”
Introduction
Alzheimer’s disease is a chronic neurodegenerative disease. It accounts for 60 to 80 percent of all dementia cases (Sosa-Ortiz, Acosta-Castillo, & Prince, 2012, 603). Alzheimer’s patients experience a progressive decline in cognitive functions and an eventual deterioration of memory. Alzheimer’s disease and related dementias result in significant social, economic, and health costs for patients, individuals, and the health system.
Clinical symptoms of Alzheimer’s are primarily diagnosed in the elderly. Health experts have identified risk factors for dementia as non-modifiable or modifiable. Non-modifiable risk factors include older age and a family history of dementia (Sosa-Ortiz et al., 2012). Modifiable risk factors include education and occupational attainment, such cardiovascular risk factors as smoking, hypertension, diabetes, and obesity, and such lifestyle and psychosocial factors as depression, physical activity, and alcohol consumption (Sosa-Ortiz et al., 2012). However, most doctors agree that such risk factors do not provide sufficient sensitivity or specificity to serve as diagnostic markers (Reitz et al., 2011). No definitive diagnostic test exists for Alzheimer’s. In living patients, an Alzheimer’s diagnosis is based only on clinical examinations and can only be confirmed postmortem upon autopsy (Reitz et al., 2011).
According to the Alzheimer’s Association, 5.3 million people in the United States have Alzheimer’s disease, with one new case developing every 67 seconds.
Nevertheless, early diagnosis of Alzheimer’s is crucial for determining appropriate interventions as the disease progresses (Bynum, 2014). While the whole brain begins to change in the first stage of Alzheimer’s, the individual does not experience any symptoms (Bynum, 2014). The next stage is referred to as early Alzheimer’s or Mild Cognitive Impairment (MCI). An individual with MCI has symptoms that do not interfere with daily activities but affect higher-level cognitive activities. In the final stage of Alzheimer’s, the patient becomes dependent on caregivers for such basic functions as feeding and using the toilet (Bynum, 2014).
The most recent estimate of Alzheimer’s total annual costs in the United States was $157-215 billion for patients over seventy, including both formal and informal care (Bynum, 2014, 535). By 2040, this cost is projected to increase to $1.2-1.6 trillion (Bynum, 2014, 535). Dementia patients have chronic needs and require increasing support over time from health and social care systems, as well as family caregivers (Fox et al., 2013). In the United States, Alzheimer’s is the sixth leading cause of death (Centers for Disease Control and Prevention, 2014).
According to the Alzheimer’s Association, 5.3 million people in the United States have Alzheimer’s disease, with one new case developing every 67 seconds (Latest Facts and Figures Report, 2015). By 2050, 13.8 million Americans will have Alzheimer’s disease (Hebert et al., 2013). The Alzheimer’s Association reports that in North Carolina, almost 160,000 people live with Alzheimer’s. That number is expected to increase to 210,000 by 2025 (Alzheimer’s disease Facts and Figures, 2015). Almost two-thirds of people with Alzheimer’s are women (Hebert et al., 2013). Women may have a higher risk of the disease, or it may be associated with longer female life expectancy (Hebert et al., 2001).
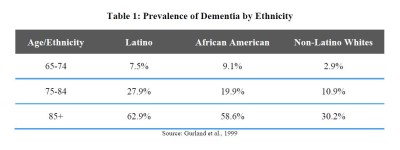
Several studies have not found significant results indicating that women have a higher risk of developing the disease. Other studies have found that women develop Alzheimer’s at a higher rate due to life experiences or biological or genetic variations (Carter et al., 2012). As the table below shows, prevalence rates of dementia are higher among Latinos and African Americans. According to Gurland et al., the prevalence of dementia among individuals between 75 and 84 years old is 9 percent higher for African Americans than non-white Latinos, it is 17 percent higher for Latinos than non-Latino whites. As age increases, the prevalence difference between Latinos and African Americans compared to non-Latino whites also increases. Latinos aged 85 years or older show 30 percent higher rates of Alzheimer’s than non-Latino whites (Gurland et al., 1999).
However, once age and educational attainment are taken into account, there are no ethnoracial differences (Gurland et al., 1999). One possible explanation is that Latino and African American patients often receive delayed diagnosis or inadequate treatment. Other factors that might account for the differences in prevalence of Alzheimer’s include perceptions of what is normal for aging, stigmas surrounding dementia, and lack of access to medical care. 2
|
Note: Here is information about this student project, provided by the Duke Sanford School of Public Policy. This student presentation was prepared during the spring of 2015 in partial completion of the requirements for PUBPOL 804, a course in the Master of Public Policy Program at the Sanford School of Public Policy at Duke University. The research, analysis, policy alternatives, and recommendations contained in this report are the work of the student team that authored the report, and do not represent the official or unofficial views of the Sanford School of Public Policy or of Duke University. Without the specific permission of its authors, this report may not be used or cited for any purpose other than to inform the client organization about the subject matter. The authors relied in many instances on data provided to them by the client and related organizations and make no independent representations as to the accuracy of the data. |
- Excerpts taken from an interview with Mr. Cubine, February 21, 2015. ↩
- Works Cited
ACT on Alzheimer’s. (2014). Retrieved February 17, 2015, from ACT on Alzheimer’s: http://actonalz.org/Alzheimer Europe. (2013). P8. Dementia-friendly communities. Retrieved February 19, 2015, from
Alzheimer Europe: http://www.alzheimer-europe.org/Conferences/Previousconferences/ 2013-St-Julian-s/Detailed-programme-abstracts-and-presentations/P8.-Dementia-friendly-communitiesAlzheimer’s Association “State Alzheimer’s Disease Plans.” (2015, February 1). Retrieved February
20, 2015, from http://act.alz.org/site/DocServer/STATE_AD_PLANS.pdf?docID=4641Alzheimer’s Association. (2011). The National Alzheimer’s Project Act.” Alzheimer’s Association,
2014. Retrieved April 9, 2015, from http://napa.alz.org/Alzheimer’s Association. (2014). “National Plan to Address Alzheimer’s Disease,” Alzheimer’s
Association, 2014. Retrieved April 9, 2015, from http://act.alz.org/site/DocServer/NatlPlan.pdf?docID=5568Alzheimer’s Association. (2015) 2015 Alzheimer’s disease Facts and Figures. Alzheimer’s
Association. Retrieved April 9, 2015, from http://www.alz.org/facts/downloads/facts_figures_2015.pdfAssistant Secretary for Planning and Evaluation. (2014). National Alzheimer’s Project Act. U.S.
Department of Health and Human Services, 2014. Retrieved April 9, 2015, from http://aspe.hhs.gov/daltcp/napa/Bratts-Brown, W. (2013, December 27). Memorandum: CAP/DA Slot Utilization and Waitlist Management. Retrieved April 8, 2015, from http://www.ncdhhs.gov/dma/cap/CAPDA_Slot_Utilization_Waitlist_Mgmt.pdf
Bynum, J. (2014). The Long Reach of Alzheimer’s disease: Patients, Practice, And Policy. Health Affairs, 33(4), 534-540. Retrieved February 2, 2015, from http://content.healthaffairs.org.proxy.lib.duke.edu/content/33/4/534.full
Carter, Christine L., Resnick, Eileen M, Mallampalli, Monica, Kalbarczyk, Anna. (2012) Sex and Gender Differences in Alzheimer’s disease: Recommendations for Future Research. Journal of Women’s Health 21(10): 1018-1023.
Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999-2013 on CDC WONDER Online Database, released October 2014. Data are from the Compressed Mortality File 1999-2013 Series 20 No. 2S, 2014, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/cmf-icd10.html on Apr 5, 2015 2:14:16 PM
Centers for Disease Control and Prevention. Healthy Aging: Alzheimer’s Disease. Retrieved April 17, 2015 from http://www.cdc.gov/aging/aginginfo/alzheimers.htm
Chin, Alexander L., Selamawit Negash, and Roy Hamilton. (2011) Diversity And Disparity In Dementia. Alzheimer Disease & Associated Disorders 25(3): 187-195.
Facilities with Special Care Units. (2015, March 16). Retrieved March 20, 2015, from http://www.ncdhhs.gov/dhsr/acls/pdf/sculist.pdf
Foldes, S. and Long, K (2014, May).The Minnesota Economic Model of Dementia: Demonstrating Healthcare Cost Savings with the New York University Caregiver Support Intervention. Retrieved April 11, 2015, from
http://actonalz.org/sites/default/files/documents/MN%20Economic%20Model%20of%20De mentia%20White%20Paper%20Final.pdfFox, C., Maidment, I., Mooniz-Cook, E., White, J., Thyrian, J. R., Young, J., et al. (2013). Optimising primary care for people with dementia. Mental Health in Family Medicine. 10 (3), 143–151.
Gaugler, J. E., Yu, F., Davila, H. W., & Shippee, T. (2014). Alzheimer’s disease And Nursing Homes. Health Affairs, 33(4), 650-657. http://content.healthaffairs.org.proxy.lib.duke.edu/content/33/4/650.full.pdf+html
Georgia Department of Human Services “Georgia Alzheimer’s Disease and Related Dementias State Plan.” (2014, June 23). Retrieved February 19, 2015, from https://gov.georgia.gov/sites/gov.georgia.gov/files/related_file/document/SB%2014.pdf
Grant launches collaborative effort to combat Alzheimer’s (2015). Retrieved April 11, 2015, from http://dukeforward.duke.edu/article/grant-launches-collaborative-effort-to-combatalzheimers.
Group Homes/Special Care Units. (2013, March 6). Retrieved February 17, 2015, from http://www.wral.com/news/state/nccapitol/asset_gallery/11998359/
Gurland, Barry J.; Wilder, David E.; Lantigua, Rafael; Sterm, Yakov; Chen, Jiming; Killeffer, Eloise H.P., Mayeux, Richard. (1999). Rates of dementia in three ethnracial groups. International Journal of Geriatric Psychiatry, 14, 481-493.
Hampel, H., Frölich, L., Hoffman, W., Prvulovic, D., Riepe, M. W., Stefan, T., et al. (2011). The future of Alzheimer’s disease: The next 10 years. Progress in Neurobiology, 95, 718–728.
Hebert, L. E. (2001). Is The Risk Of Developing Alzheimer’s disease Greater For Women Than For Men? American Journal of Epidemiology 153 (2), 132-136.
Hebert, Liesi E.; Weuve, Jennifer; Scherr; Paul A., et al. (2013, February 6). Alzheimer disease in the United States (2010−2050) estimated using the 2010 census. Neurology published online. DOI: DOI 10.1212/WNL.0b013e31828726f5
a. Hoban, R. (2012, November 4). Rate Cuts Threaten Dementia Care Facilities. Retrieved February 17, 2015, from http://www.northcarolinahealthnews.org/2013/11/04/rate-cuts-threatendementia- care-facilities
b.Hoban, R. (2012, December 14). Alzheimer’s Patients Caught Up in State Medicaid Service Changes. Retrieved February 17, 2015, from http://www.northcarolinahealthnews.org/2012/12/14/alzheimers-patients-caught-up-in-statemedicaid- service-changes/
Hoban R. (2013, February 4). No Fix in Sight Yet for Alzheimer’s Special Care Units. Retrieved April 28, 2015, from http://www.northcarolinahealthnews.org/2013/02/04/no-fix-in-sightyet- for-alzheimers-special-care-units/
Hoban, R. (2013, June 11). House & Senate Budgets Compared. Retrieved April 7, 2015, from http://www.northcarolinahealthnews.org/2013/06/11/house-senate-budgets-compared/).Hoban, R., Singh, J., &
Namkoong, H. (2014, August 1). Hospitals, Adult Care Homes Big Losers in Budget. Retrieved February 17, 2015, from http://www.northcarolinahealthnews.org/2014/08/01/hospitals-adult-care-homes-big-losersin- budget/
Hoban, R., Singh, J., & Namkoong, H. (2015). FINAL: The Health and Human Services Budgets Compared. Retrieved February 17, 2015, from http://www.northcarolinahealthnews.org/thehealth- and-human-services-budgets compared/
In the Public Interest. “North Carolina Mental Health System.” (2015). Retrieved April 29, 2015,
from http://www.inthepublicinterest.org/case/north-carolina-mental-health-systemKelly, C., & Williams, I. (2007). Providing Dementia-Specific Services to Family Caregivers: North Carolina’s Project C.A.R.E. Program. Journal of Applied Gerontology, 26(4), 399-412. Retrieved February 18, 2015, from http://www.ncdhhs.gov/aging/ad/Providing_Dementia- Specific_Services.pdf
Land of Sky Regional Council: Project C.A.R.E. (2012). Retrieved April 8, 2015, from http://www.landofsky.org/projectcare
Leslie, L., & Morgan, D. (2012, December 13). Medicaid benefit cuts impact thousands of Alzheimer’s patients. Retrieved February 17, 2015, from http://www.wral.com/medicaidbenefit- cuts-impact-thousands-of-alzheimer-s-patients/11874686/
Lin, P. J., Fillit, H. M., Cohen, J. T., & Neumann, P. J. (2013). Potentially avoidable hospitalizations among Medicare beneficiaries with Alzheimer’s disease and related disorders. Alzheimer’s & Dementia, 9(1), 30-38. http://www.sciencedirect.com/science/article/pii/S1552526012025204
Long, K. H., Moriarty, J. P., Mittelman, M. S., & Foldes, S. S. (2014). Estimating The Potential Cost Savings From The New York University Caregiver Intervention In Minnesota. Health Affairs, 33 (4), 596-604.
Mastry, Olivia. (2015, March). Speech to the North Carolina Taskforce on Alzheimer’s disease and
Related Dementia.Miller, Debra. (2011, September). Alzheimer’s disease and Caregiving. The Council of State
Governments Knowledge Center. Retrieved April 11, 2015, from: http://knowledgecenter.csg.org/kc/content/Capitol-Research-alzheimers-disease-andcargivingMinnesota Board on Aging (2011). Preparing Minnesota for Alzheimer’s: the Budgetary, Social and Personal Impacts. Retrieved February 17, 2015, from: http://www.alz.org/national/documents/MN_state_plan.pdf
Morgan, J. (2008). Union County Community Health Assessment 2008. Retrieved April 1, 2015, from http://www.co.union.nc.us/Portals/0/Health/Documents/CHA2008.pdf
Morgan, J. (2012). Union County 2012 Community Health Assessment. Retrieved April 1, 2015, from http://www.co.union.nc.us/Portals/0/Health/Documents/CHA2012.pdf
National Alliance for Caregiving & Alzheimer’s Foundation of America. (2014). From plan to practice: Implementing the National Alzheimer’s Plan in Your State. National Alliance for Caregiving.NC PACE Association: History and Growth. (2015). Retrieved April 9, 2015, from http://ncpace.org/pace-in-nc/history-and-growth
NC PACE Association: PACE Sites. (2015). Retrieved April 9, 2015, from http://ncpace.org/pace-innc/ pace-sites
North Carolina Community Alternatives Program for Disabled Adults Waiver (CAP/DA) (2014, March). Retrieved April 7, 2015, from http://www.payingforseniorcare.com/medicaidwaivers/ nc-community-alternatives-program for-disabled-adults.htmlNorth Carolina Department of Health and Human Services. “Facilities with Special Care Unit Beds.” (2015, April 16). Retrieved April 29, 2015, from http://www.ncdhhs.gov/dhsr/acls/pdf/sculist.pdf
North Carolina Division of Aging and Adult Services: Home and Community Care Block Grant (2013, March 14). Retrieved April 9, 2015, from http://www.ncdhhs.gov/aging/manual/hccbg/hccbg.htm
North Carolina Medicaid Special Bulletin: Cap Limits on PACE Enrollments for State Fiscal Year 2014 (2014, May). Retrieved April 10, 2015, from http://www.ncdhhs.gov/dma/bulletin/pdfbulletin/0514_Special_Bulletin_PACE.pdf
North Carolina Mental Health System. (2015). In the Public Interest. Retrieved April 10, 2015, from http://www.inthepublicinterest.org/case/north-carolina-mental-health-system
North Carolina’s Family Caregiver Support Program. (2014, December 11). Retrieved February 1, 2015, from http://www.ncdhhs.gov/aging/fchome.htm
Oakes, A. (2013, September 3). NC continues stopgap funding for group homes. Retrieved February 17, 2015, from http://www.wataugademocrat.com/news/nc-continues-stopgap-funding-forgroup- homes/article_1b33c8c6-e796-5614-804f-2977c120412a.html
Reauthorize the Older Americans Act. (2015, March 1). Retrieved April 8, 2015, from http://www.aarp.org/politics-society/advocacy/info-2014/where-aarp-stands-older-americansact.html
Reinhard, S., Feinberg, L., Choula, R. (2012). A Call to Action: What Experts Say Needs to be Done to Meet the Challenges of Family Caregiving. AARP Public Policy Institute. Retrieved April 11, 2015, from Reitz, C., Brayne, C., & Mayeux, R. (2011). Epidemiology of Alzheimer disease. Nature Reviews Neurology, 7, 137-152.
Senate Bill 466 (2015). Retrieved April 11, 2015, from http://www.ncleg.net/gascripts/BillLookUp/BillLookUp.pl?Session=2013&BillID=s466
Shaw, L. (2013). Response to NC Department of Health and Human Services Division of Medical Assistance Request For Information RFI-DMA 100-13. Retrieved April 8, 2015, from http://ncpace.org/images/uploads/NC_PACE-DMA100-13_FINAL.pdf
Social Worker (BSW) Salaries. (2015). Retrieved April 11, 2015, from http://www.payscale.com/research/US/Job=Social_Worker_(BSW)/Salary#CareerPaths
Sosa-Ortiz, A., Acosta-Castillo, I., & Prince, M. J. (2012). Epidemiology of Dementias and Alzheimer’s disease. Archives of Medical Research, 43, 600-608. ↩